Welcome to the first instalment of our blog series on injury prevention and recovery at HealthFix. In this blog, we’ll focus on a critical aspect of your well-being: ankle health. Whether you’re an athlete aiming for peak performance or someone seeking to regain function, understanding the significance of ankle health and the role of comprehensive rehabilitation is paramount. Ankles are one of the most poorly rehabbed joints in the body, with chronic ankle instability a common occurrence after an ankle injury, so knowing how best to take care of your ankle and how best to recover from an injury is super important.
The Ankle’s Vital Role
The ankle is a remarkable joint responsible for bearing weight, ensuring stability, and facilitating movement. However, it’s also prone to various injuries, with lateral ankle sprains being a common occurrence.
Chronic Ankle Instability: An Ongoing Challenge
Ankle injuries are, unfortunately, a common occurrence, and they often have long-lasting implications for those who experience them. One of the most persistent and challenging issues that can arise from an ankle injury is chronic ankle instability. This condition can be particularly frustrating and debilitating, and it frequently stems from incomplete or inadequate rehabilitation following the initial injury. Understanding chronic ankle instability and its impact on daily life and physical activities is crucial for anyone who has experienced or is currently dealing with this condition.
The Impact on Daily Life
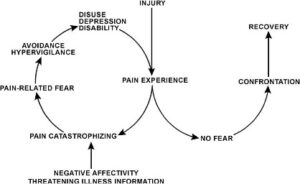
The repercussions of chronic ankle instability can extend far beyond the physical realm. For those affected, it can significantly impact their daily lives. Simple tasks such as walking, climbing stairs, or standing for extended periods may become challenging. The fear of the ankle giving way can also lead to a decrease in confidence and an increased risk of falls. This can limit one’s independence and overall quality of life.
Participation in Physical Activities
In addition to daily life, chronic ankle instability can hinder an individual’s ability to engage in physical activities. This is particularly frustrating for those who lead an active lifestyle or participate in sports and recreational activities. The recurring pain and instability can lead to a reluctance to participate, fear of re-injury, and a decline in overall fitness.
Moreover, without proper treatment and rehabilitation, chronic ankle instability can set the stage for further injuries. As the ankle struggles to support the body’s weight and maintain balance, the risk of sustaining new injuries to the ankle or other parts of the body, such as the knee or hip, increases.
The Importance of Rehabilitation
Understanding the long-term consequences of chronic ankle instability underscores the importance of comprehensive rehabilitation after an ankle injury. Incomplete rehabilitation is a significant risk factor for this condition. Adequate rehabilitation not only facilitates the healing process but also strengthens the ankle, improving its ability to withstand future stresses. A skilled physiotherapy team can create a tailored rehabilitation program to address each patient’s unique needs, ensuring a more complete and robust recovery.
Comprehensive Rehabilitation at HealthFix
At HealthFix, we are committed to empowering individuals to overcome ankle injuries and regain strength and confidence to return to sport or even just to be able to enjoy whatever life brings. Our approach to ankle rehabilitation is not just about healing; it’s about preventing future injuries.
What can you expect?
Initial Evaluation: The rehabilitation process begins with a thorough evaluation by a physiotherapist. They will assess the extent of the instability, any associated pain or discomfort, and the range of motion in the ankle.
Individualised Exercise Regimen: Based on the evaluation, a customised exercise regimen is created to address the specific weaknesses and imbalances contributing to ankle instability. This program often includes exercises to strengthen the muscles around the ankle and improve balance and proprioception. Common exercises may include:
-
Strengthening Exercises: These exercises target the muscles in the lower leg, such as the calf muscles and the muscles on the front of the shin. They may include calf raises, resistance band exercises, and exercises that involve ankle movements.
-
Balance and Proprioception Training: Balance exercises, such as single-leg stands and wobble board exercises, are crucial for improving the body’s awareness of its position in space and enhancing stability.
-
Range of Motion Exercises: Gentle stretching and range of motion exercises help improve the flexibility of the ankle joint. This is important for preventing stiffness and maintaining proper function.
-
Functional Training: Rehabilitation will include functional exercises that mimic activities the individual encounters in daily life or sports. This might involve walking, jogging, jumping, and pivoting exercises to simulate real-life situations.
Manual Therapy: In some cases, a physiotherapist may use manual therapy techniques, such as joint mobilisation or soft tissue massage, to alleviate pain, improve range of motion, and restore normal joint mechanics.
Patient Education: An important aspect of rehabilitation is educating the patient about their condition, proper footwear, and strategies to prevent re-injury. This includes guidance on when and how to return to sports or other physical activities safely.
Progressive Overload: The rehabilitation program should be progressive, gradually increasing the intensity of exercises and challenges as the patient’s strength and stability improve.
Monitoring and Adjustments: Regular follow-up appointments to monitor progress and make adjustments to the rehabilitation program as needed.
Functional Testing: Functional tests will be conducted to assess the individual’s readiness to return to their desired activities or sports safely.
Expert Leadership
Our programs are led by Titled Sport and Exercise Physiotherapists Caitlan and Sean.
Sean also serves as the NSW Institute of Sport’s Performance Health Manager, and brings a wealth of experience and expertise to our team.
Caitlan is the Head Physio and Strength and Conditioning Coach for an A League Women’s Football team and knows how to get you back efficiently.
Your Partner in Rehabilitation
Just as in our previous blog, HealthFix remains your partner in the pursuit of wellness. We’ve developed fixed-price rehabilitation programs that are carried out in our high-performance facility by our esteemed multi-disciplinary team.
A High-Performance Environment
Our facility mirrors a high-performance environment, equipped with a skilled integrated team and a cutting-edge gym. We provide you with the tools, guidance, and support needed to navigate the path to recovery successfully.
Commitment to Positive Outcomes
Our rehabilitation programs are designed with the sole purpose of achieving positive outcomes for you. We understand that injury management is not just about healing; it’s about ensuring your safe return to all activities.
Conclusion
Ankle injuries can present significant challenges, but with the right approach to rehabilitation and the support of the HealthFix team, you can emerge stronger than ever. Stay tuned for more blogs in our series, where we’ll delve into other common injuries and their paths to recovery. Together, we’ll work towards a pain-free and confident return to the activities you love.