by Ash Cooney | Conditions, Personal Training
Increasing your running load, with regards to training for a big event, can be both exciting and challenging, but also something that requires preparation, thought and balance. The human body will generally have a significant response to an overly quick and intense...
by Ash Cooney | Conditions, Latest News, Physiotherapy
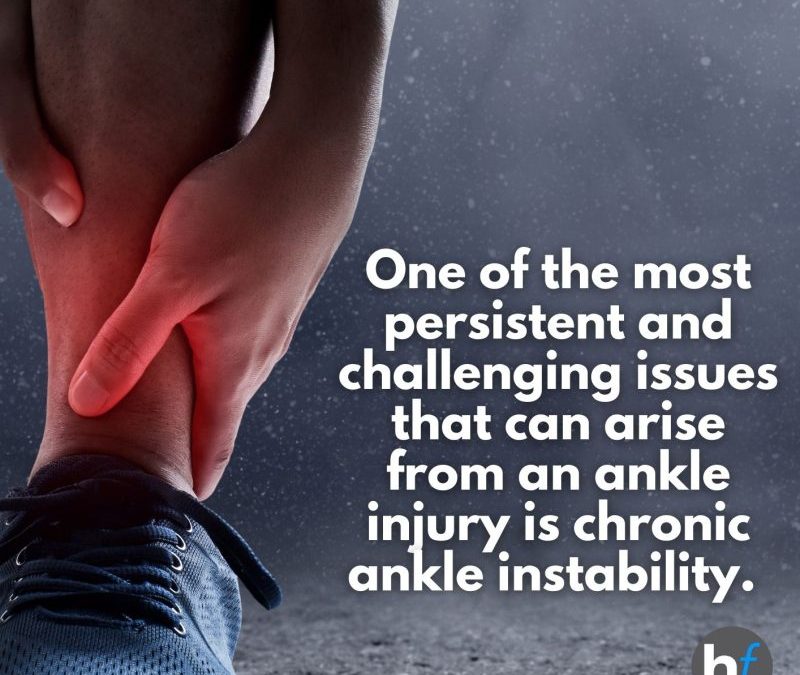
Welcome to the first instalment of our blog series on injury prevention and recovery at HealthFix. In this blog, we’ll focus on a critical aspect of your well-being: ankle health. Whether you’re an athlete aiming for peak performance or someone seeking to...

by Ash Cooney | Conditions
Maintaining and prioritising healthy bones is essential for a vibrant and active life. Bones provide the framework that supports our bodies and allows us to move freely. Unfortunately, many individuals overlook the importance of bone health until they face conditions...

by Ash Cooney | Conditions, Latest News
Exploring All Things Diabetes with Dr. Devina Joshi: Expert Insights for Optimal Management At Healthfix we are passionate about empowering our community with valuable information and resources for a healthier and happier life. Today, we are excited to share an...

by Ash Cooney | Conditions, Physiotherapy
Living in a sports-loving nation like Australia, it’s no surprise that many individuals, both athletes and non-athletes, turn to sports as a means of recovery after surgery. However, successful rehabilitation requires a proactive and preventative approach,...

by Ash Cooney | Conditions, Physiotherapy
Living with chronic musculoskeletal pain can be a challenging and overwhelming experience. It often affects various aspects of your life, making it difficult to perform daily activities and participate in the things you enjoy. As someone seeking relief from this pain,...