by admin | Latest News, Promotions
Are you ready to embark on a transformative journey to a healthier, stronger, and revitalised version of yourself? Healthfix is delighted to introduce the New Year Challenge, our 8-Week Reboot. The Reboot is a powerful program designed to cater to diverse health needs...

by Ash Cooney | Latest News
The holiday season is upon us, and amidst the festive cheer and indulgent treats, maintaining your fitness routine can be a challenge. At Healthfix, we’re here to make sure you not only survive but thrive during the holidays with our Exercise Survival Guide,...

by Ash Cooney | Latest News
In the ever-evolving landscape of health and fitness down under, one trend is poised to dominate in 2024 like never before – the explosive surge in strength training. Over the past decade, it’s quietly been transforming lives, and now, it’s set to take...
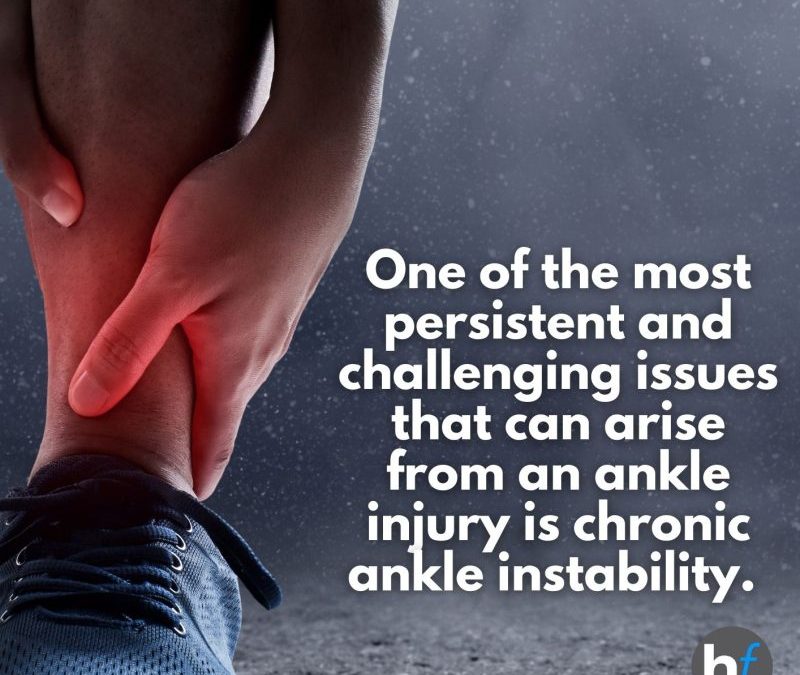
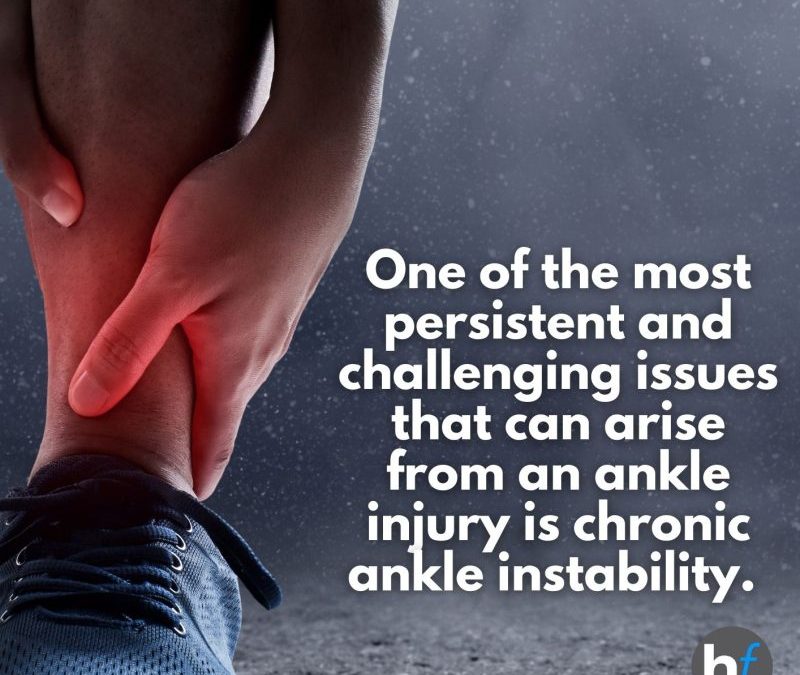
by Ash Cooney | Conditions, Latest News, Physiotherapy
Welcome to the first instalment of our blog series on injury prevention and recovery at HealthFix. In this blog, we’ll focus on a critical aspect of your well-being: ankle health. Whether you’re an athlete aiming for peak performance or someone seeking to...

by Ash Cooney | Latest News
By Caitlan Skillicorn, Senior Physiotherapist on behalf of the Healthfix Physiotherapy team Hello, Healthfix Community! At Healthfix, we’re committed to your well-being and providing the best care possible. Today, we want to share our perspective on a recent...
by Ash Cooney | Latest News
Are you ready to unlock the secrets of staying healthy, performing at your best, and preventing injuries and illnesses? Healthfix is thrilled to invite you to our upcoming event that promises to revolutionise your approach to health and wellness. 📆 Date:...