Did you set a big goal for yourself this year?
Perhaps it was to improve your overall health, achieve a specific fitness milestone, or simply feel more energised and alive. You started with immense motivation and determination, envisioning a healthier and happier version of yourself. But then, life happened. Work demands, family responsibilities, stress, and sleepless nights started to chip away at your enthusiasm. These challenges are real, and they affect us all. However, they don’t have to be insurmountable barriers to your well-being.- What if you could bring conscious awareness to your daily habits and learn how to align them with your life’s demands?
- What if you could identify the obstacles standing in your way and develop strategies to overcome them?
- What if you could live in harmony with your core values, propelling you toward your highest good?
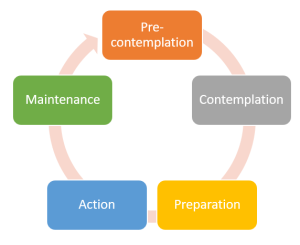
The Stages of Behaviour Change
Before we explore the profound impact of coaching, it’s essential to understand the stages of change. Change is not a linear process; rather, it’s a journey filled with ups and downs. Prochaska and DiClemente’s Transtheoretical Model identifies five stages:- Pre-contemplation: At this stage, you might not yet recognise the need for change. You may be unaware of the health issues or habits that require attention.
- Contemplation: In this phase, you acknowledge the need for change and start considering your options. You weigh the pros and cons of taking action.
- Preparation: You’re ready to take action, and you may even have a plan in place. You’re determined to make changes in your life.
- Action: This is where you put your plan into motion. You actively modify your habits and behaviours to achieve your wellness goals.
- Maintenance: You’ve made significant progress, and now your focus is on sustaining these changes over the long term.
How Health and Wellness Coaching Facilitates Change
Health and wellness coaching aligns perfectly with these stages of change. Here’s how coaching can be your compass on your wellness journey:
- Pre contemplation: A coach helps you become aware of your health and well-being. They create a safe space for self-reflection and exploration.
- Contemplation: Your coach supports you in clarifying your goals and values. Together, you identify what truly matters to you and what you’re willing to change.
- Preparation: Coaches assist you in creating a personalised plan, breaking down your goals into manageable steps. They provide guidance and motivation.
- Action: During this phase, a coach serves as your accountability partner. They help you stay on track, provide encouragement, and adjust your plan as needed.
- Maintenance: Even after you’ve achieved your initial goals, a coach continues to work with you to ensure long-term success. They help you navigate any setbacks and celebrate your victories.
The Benefits of Health and Wellness Coaching
- Personalised Guidance: Coaching is not one-size-fits-all. Your coach tailors their approach to your unique needs and circumstances.
- Accountability: A coach keeps you accountable for your commitments, helping you stay motivated and on course.
- Empowerment: Through coaching, you learn to take control of your health and well-being, making informed choices aligned with your values.
- Lifestyle Integration: Coaches help you integrate healthier habits seamlessly into your daily life, making wellness a sustainable part of who you are.
- Mindset Transformation: Coaching fosters a growth mindset, helping you overcome self-limiting beliefs and replace them with empowering thoughts.